Researchers
Dr. Elisia L. Cohen (Department of Communication, University of Kentucky)
Dr. Robin C. Vanderpool (College of Public Health, University of Kentucky)
Bethney Wilson, MA (Department of Communication, University of Kentucky)
Purpose
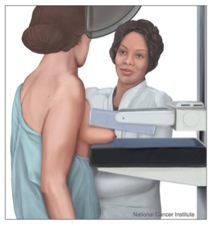
Breast cancer is one of the most common cancers among women. In 2012, approximately 39,920 women will die from breast cancer, and approximately 1 in 3 cancer diagnoses in women will be breast cancer (American Cancer Society, 2012). Breast cancer screening guidelines recommend biennial mammography screening for women aged 50 to 74 (U.S. Preventative Task Force, 2009). In Kentucky, an estimated 3,160 new cases of breast cancer will be diagnosed in 2012 and an estimated 570 people will die from breast cancer (American Cancer Society, 2012). Rural Appalachian Kentucky communities are disproportionately affected by high incidences of cancer and are traditionally underserved by the healthcare system (Hall, Uhler, Coughlin, & Miller, 2002; Wingo et al., 2008). Women in rural Appalachian Kentucky do not exhibit higher breast cancer incidence (60.34 per 100,000 people) than women in other areas of Kentucky (statewide 65.84 per 100,000 people). However, there are disparities in mortality rates with the age-adjusted breast cancer mortality rate for women in Appalachian Kentucky (13.19 per 100,000 people) as higher than the Kentucky (including Appalachia, statewide 13.12 per 100,000 people) region (Kentucky Cancer Registry, 2012).
A paucity of research has examined barriers to timely mammography screening, diagnostic screening, and appropriate follow-up treatment among Appalachian women; these barriers may be responsible for higher breast cancer mortality rates among Appalachian women.
Practical Implications
In the breast cancer context, Andrews (2001) suggested that the interpersonal skills of mammography technicians influences the intentions of the patients, suggesting that further study was needed to evaluate the link between mammography technician communication skills and patient perceptions of pain. Similarly, Carney et al. (2002) found that women who reported communication competence, specifically that the mammography technician adequately talked them through the procedure, were more likely to adhere to mammography guidelines. The question remains, in the context of Appalachian women residing in a medically underserved community, whether mammography experiences and communication with providers about breast cancer screenings are identified as barriers to future mammography screening adherence. The purpose of this study is to determine what specific barriers women residing in Appalachian Kentucky report.
Publications or Presentations
Cohen, E.L., Wilson, B.R., Vanderpool, R.C., & Collins, T. Barriers to patient-centered mammography among Appalachian Kentucky women. International Communication Association Annual Conference. June 20th, 2013. London, UK.
Cohen, E.L., Wilson, B.R., Vanderpool, R.C., & Collins, T. Identifying adherence barriers to screening mammography recommendations among Appalachian Kentucky women. 34th Annual Meeting & Scientific Sessions: Rapid Communications. Society of Behavioral Medicine. March 20, 2013. San Francisco, CA.
References
American Cancer Society. (2012). Cancer facts and figures, 2012. Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf
Andrews, F. J. (2001). Pain during mammography: Implications for breast screening programs. Australasian Radiology, 45, 113-117.
Carney, P. A., Harwood, B. G., Weiss, J. E., Eliassen, M. S.,& Goodrich, M. E. (2002). Factors associated with interval adherence to mammography screening in a population-based sample of New Hampshire women. Cancer, 95(2), 219-227.
Kentucky Cancer Registry. (2013). kcr.uky.edu
U.S. Preventative Task Force. (2009). Screening for breast cancer. Retrieved from http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm
External Website
University of Kentucky College of Public Health Rural Cancer Prevention Center